This post also appeared on JSI’s website.
“It’s a ghost! It’s a ghost,” they yelled.
Charlotte Mujawayezu, a farmer and mother of four from Nyamiyaga, Rwanda, was going to buy sugar when she heard voices from the forest. Curious, she approached a crowd of people to catch a glimpse of what all the shouting was about.

But what she saw was much more distressing than a ghost: an abandoned newborn baby lay in the dust, his clothes torn and dirty, and his body terribly thin.
“He looked old enough, but he couldn’t speak nor walk,” Charlotte said. “His face was so scary that nobody in the crowd could approach or touch him.”
But Charlotte felt pity when she looked at the child. Despite living in already crowded conditions – two rented rooms for herself, her husband, and three children – she immediately took the infant home to change his clothes, then rushed him to Nyamiyaga Health Center.
“People were laughing at me, but I knew it was a blessing for me,” she said. “That is why I named the child Mugisha, to mean blessing.”
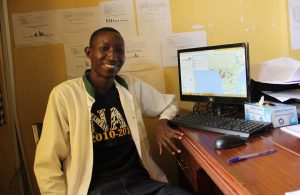
At the health center, Mugisha was transferred to Remera Rukoma Hospital, where he was received by Dr. Deo Rugabano. Trained by MCSP on Integrated Management of Childhood Illness (IMCI), he identified the boy as suffering from malnutrition and dehydration.
“Mugisha was yawning every time, but he couldn’t cry since he hadn’t energy anymore,” Dr. Deo said.
With the infant unable to drink, Dr. Deo knew to begin an intravenous infusion and oral rehydration salt solution simultaneously. Every two hours thereafter, Dr. Deo checked the boy until his hydration improved. Then he moved Mugisha to the care of the hospital’s nutritionists.
Dr. Deo is one of 56 Rwandan providers trained by MCSP to identify, assess and treat illnesses in children under five. These district trainers then provide training and mentorship in health centers across 10 Program supported districts. To date, the Program has trained more than 529 health providers on IMCI to develop strong links between facility- and community-based services and the health system.
These efforts are part of MCSP’s global efforts to end preventable child deaths – including the 45% of child deaths linked to malnutrition. In countries like Rwanda, we’re working to protect children from diseases and to improve their access to lifesaving treatments. This includes building capacity to plan, leverage resources, and scale up high-impact, cost-effective child health interventions. And it means extending child health services to hard-to-reach populations and those with limited access to services.

MCSP’s successes are built one person at a time. In the case of Mugisha, the story has a very happy ending. After three weeks of hospital care, he was healthy enough to be sent home with Charlotte. And as the authorities continue to search for Mugisha’s birth parents – and Charlotte continues the process to legally adopt him – he remains a thriving, vibrant boy.
“It is a shame to people who were saying Musisha was a ghost,” Charlotte said. “Now he is a normal child, he hasn’t any problem.”
“I am really blessed,” she adds.

