MCSP’s own Vikas Dwivedi co-authored the blog below on the link between improving health outcomes and developing health information systems that “predictably, reliably, and securely” make patient data and other information portable and available. This post originally appeared on the Routine Health Information Network website.
By: Alpha Nnsaghurwe, Chris Wright, Vikas Dwivedi, Nosa Orobaton, Michael Stelmach, Moses Busiga
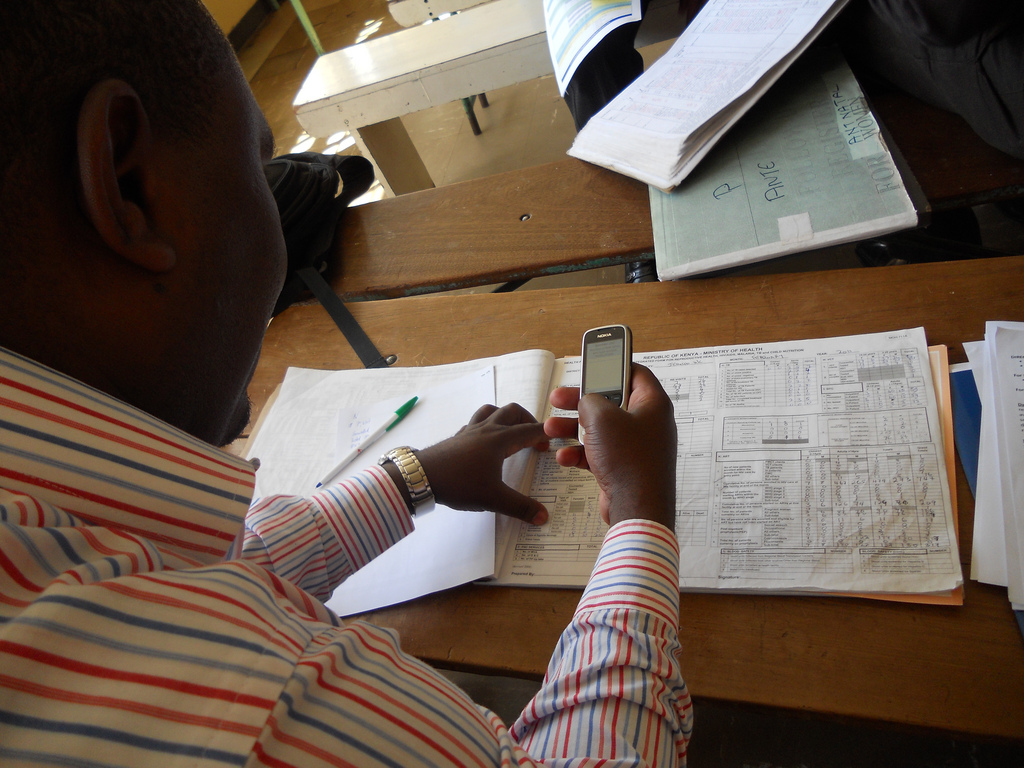
Well-performing health information systems (HIS) are a crucial catalyst for improving health outcomes and health system performance. Countries and development partners have made progress in strengthening data collection and deploying technologies to move data up the health system for monitoring and evaluating performance. But to realize the transformative power of information, it is the frontline healthcare workers—the doctors, nurses, community health workers, etc.—who require information to make informed, intelligent decisions. This includes patient data across the continuum of care; and information systems that enable smooth and timely client referrals, prompt recognition of and support to indigent clients, and routine supply of essential medicines and other health commodities. Additionally, providing information in the hands of citizens on availability of services at health facilities, quality of healthcare, and follow-up on personal care can improve health seeking decisions.
The challenge is to design HIS that predictably, reliably, and securely makes patient data and other information portable and available across different facilities, locations, and levels of care. This flow of data should support clients’ continuity of HIV treatment across public or private health facilities, and enable a pregnant woman to obtain her next dose of SP to prevent malaria regardless of where she is served. Usable information in the hands of healthcare workers is the single most important objective of any HIS; everything else is secondary.
In recent years, technological advancement has led to the introduction of a variety of digital applications to support HIS. Many are program-focused, organization-specific, or donor-driven and there are multiple software platforms and different data standards. To get data into the hands of frontline healthcare workers, these existing applications must be leveraged and new applications must be deployed within rationally designed information architecture to ensure real time access to routine, secure and quality data across the continuum of care and across all levels of the health system. The new World Bank/WHO/USAID Roadmap for Health Measurement and Accountability Post-2015 stresses that “Public health and clinical care cannot be delivered safely, with high quality, and in a cost-effective manner, without seamless, sustainable, and secure data and information exchanges at all levels of the health system.” Technologies must be able to “talk” to each other and exchange data between multiple systems, using common terminologies. In a word, they must be interoperable.
In Tanzania, the Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) has embarked on an ambitious effort to develop and deploy a Health Information Mediator for interoperability between technology solutions and to achieve the desired goal of empowering healthcare workers, at national scale. This effort, envisioned in the country’s 2013 eHealth Strategy, builds on its recent success in designing and deploying national eLMIS, DHIS2, HRHIS, and a master facilities registry. The vision (figure 1) is to enable data exchange between health domains such as electronic medical records, birth and death registries, provider and facility registries, and national health insurance funds. Central to the ministry’s strategy is its emphasis on defining objective requirements and standards to guide technology acquisition.
“The health sector is ready to embrace the rapid development of technology for improving administrative processes, patient/client recording, and communication. The Ministry is committed to guiding the development of information exchanged through interoperability of its systems.” – Mr Hermes S. Rulagirwa, head ICT unit, MoHCDGEC.
Leveraging our successful deployments of interoperability solutions for large-scale state public health programs in the US, John Snow, Inc. through the USAID-funded Maternal and Child Survival Program, is collaborating with the Government of Tanzania, development partners, and other stakeholders to introduce interoperability and to improve decision-making by frontline healthcare workers.
“As envisioned in the eHealth strategy, we have come a long way in implementing digital solutions, including development of eLMIS, DHIS2, HRHIS and the master facility registry. It is now time to enable these systems to talk to each other. We should design systems that provide continuity of care starting from pregnancy to child birth and beyond” – Mr Marcos Mzeru, ICT unit, MoHCDGEC.
In Tanzania as in India, Brasil, California, or Massachusetts, , the challenges are similar; significant variability in the technology-based systems; reliance on paper-based systems; resistance to new technologies and workflows by healthcare workers; and issues around governance of system development and management. Building integrated healthcare systems is complicated, and technology is only part of the solution. Ensuring that data is being consistently and accurately shared and that workflows are consistently followed is key to building an effective interoperability system. Technology solutions and the decision-support data they provide must be valued by users—health care workers, administrators and managers, policymakers at every level—and integrated into their routine workflows.
We are seeing a convergence in HIS and technologies around the world, with countries in the Global North and the Global South facing similar opportunities and challenges to improve how health information is used to improve health outcomes. We know that technology alone is not a panacea, but it can be a game changing enabler in strengthening a culture of data use throughout the health system.