This post also appeared on the Healthy Newborn Network website.
Dressed in scrubs, the doctor leans over the woman in labor and carefully checks that the birth is progressing normally. Satisfied, she gently tells the woman when to push. Soon the baby’s head appears and the doctor carefully delivers baby Natalie. She checks the baby to ensure that she is healthy.
The baby is perfect – perfectly plastic, that is.
Natalie is not your typical baby and this is not your typical birth. NeoNatalie, as she is officially known, is an anatomic model that is used with MamaNatalie, a birthing simulator, to create realistic training scenarios. Both play a key role in scenes like this one, at the Taunggyi Learning and Performance Improvement Center (L&PIC) in Southern Shan State of Burma, as they do throughout the country at similar training centers.
At Taunggyi L&PIC in Southern Shan State, a participant practices immediate newborn care on an anatomic model. In another center in Pathein, Ayeyarwady Region, the skills lab management team practices how to assemble simulation models. And in yet another center in Sittwe, Rakhine State, participants stitch together simulation models with locally available materials to be used during trainings.
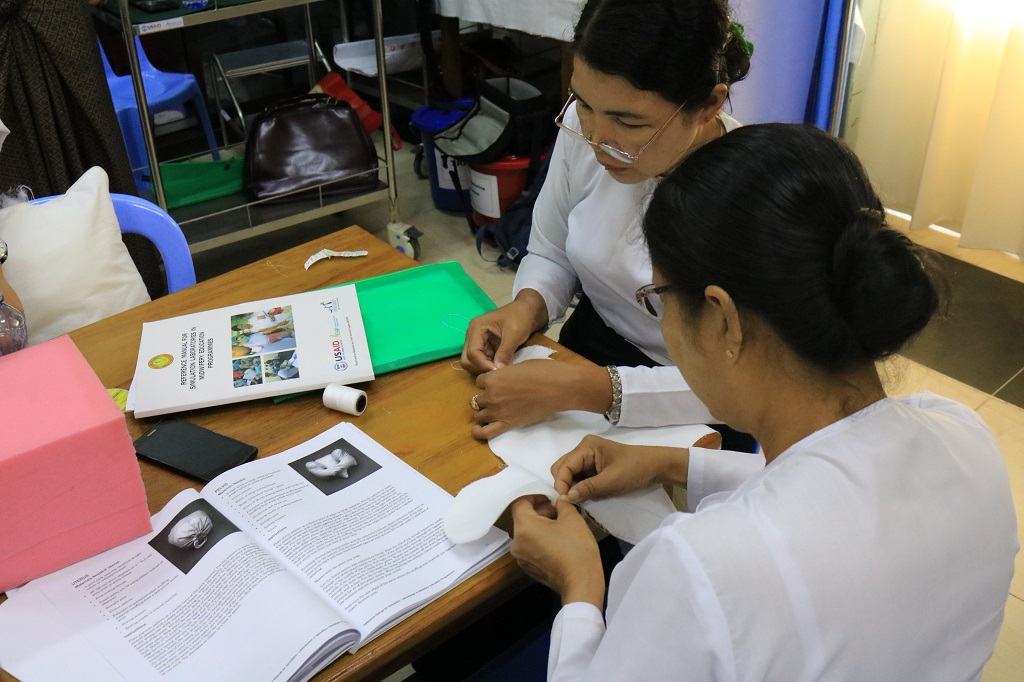
materials for use at L&PIC, Sittwe, Rakhine State.
L&PICs have so far been established in five of the country’s 14 states and regions. At each, participants strengthen skills through training sessions on normal labor and delivery; immediate newborn care; newborn resuscitation; management of severe pre-eclampsia and eclampsia; management of postpartum hemorrhage; use of a partograph; and infection prevention practices.
While pre-service education is critical, it is not the only way to ensure the quality of care delivered by Burmese doctors, nurses and midwives. These competency-based, in-service capacity-building activities are essential for providers to continue to update their knowledge and skills. “Low-dose, high-frequency” training sessions, like those offered through the L&PICs, give midwives the confidence and ability to apply and maintain newly learned skills in their day-to-day practice.
The initiative goes beyond learning hubs for professionals in each region. Many participants are part of State or Regional Health Training Teams, and take their improved skills back to their clinics or hospitals to train other providers and Township Training Teams. These efforts feed into the larger goal of improved quality of care and strengthened clinical practicum sites throughout Burma, which ultimately improves the ability of frontline health workers to effectively deliver maternal, newborn and child health services.

USAID’s flagship Maternal and Child Survival Program (MCSP) is working with the Government of Burma, through its Ministry of Health and Sports (MOHS), to strengthen the midwifery and nursing professions through improved in-service training and continuing professional education to reduce maternal and child morbidity and mortality.
MCSP is collaborating with the MOHS – and working closely with state and regional authorities – to roll out this initiative through L&PICs established in Magway, Rakhine, Ayeyarwady, Shan North, and Shan South states and regions. In partnership with these groups, MCSP also finalized learning materials to improve care on the day of birth.
The Program integrates maternal, newborn and child health in-service training at the state, regional and township levels. MCSP also supports the development of post-training follow-ups to obtain feedback from participants. This ensures that skills are being taught effectively and that participants are correctly applying their new skills and knowledge.
“These new L&PICs serve as platforms for building vital, sustainable skills for midwives, nurses and doctors,” said USAID Mission Director Teresa McGhie at a recent L&PIC launch. “This upholds the Ministry of Health and Sports’ plan to advance universal health coverage in Burma and it ensures women get the services they need.”
The value in these trainings is more than just a hunch – it has been measured. Participants, scored in pre- and post- exams to assess their competency, improved significantly after their training. On the pre-tests, average scores ranged from 24% (use of the partograph) to 80% (management of pre-eclampsia/eclampsia). In the post-test exams, average scores ranged from 91% (normal labor) to 100% (management of pre-eclampsia/eclampsia).

the simulation model at Sittwe L&PIC, Rakhine State.
The centers also save time and money. As Dr. Phyo Phyo Mon, the Skills Lab Coordinator at Shan State L&PIC, said: “If we go to Naypyitaw capital, the capital… there will be transportation costs, creating financial problems. In Shan state, those who are near the L&PIC/skills lab can practice here so it will save the time. Moreover, anybody can practice at this center.”
In Magway, newly recruited midwives are also reaping the benefits of the L&PIC. The training team there has started using the L&PIC and MCSP’s capacity-building program to strengthen the knowledge and skills of 123 midwives, providing them with technical updates before they begin their work.
The centers serve as repositories for up-to-date materials, places to apply evidence-based teaching and learning approaches, and models of government cross-departmental collaboration to improve health outcomes. Through this standardized approach, Burma’s midwives are being equipped with the skills to provide high-quality care to Burma’s people – taking their skills from NeoNatalies to real-life babies.

