This content also appeared on JSI’s website.
Ambanja district, Madagascar — “I didn’t really care about surveillance. I didn’t understand how important it was,” said Dr. Lucie Famamesamtsoa.
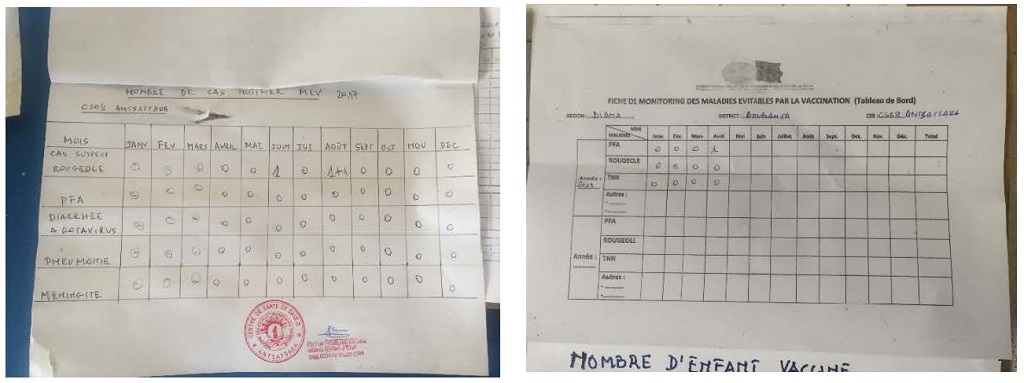
As head of the Antsatsaka Basic Health Center II in northern Madagascar, Dr. Famamesamtsoa’s days are busy. As a result, vaccine preventable disease (VPD) surveillance — including surveillance for acute flaccid paralysis (AFP) — sometimes fell through the cracks.
However, actively checking and following up on cases of AFP is fundamental to eradicating wild poliovirus and any related variants, such as vaccine-derived poliovirus, which occurred in Madagascar in 2014. By identifying children who may have symptoms of polio virus, health teams are able to determine if and where additional measures (such as polio campaigns or further routine immunization strengthening efforts) are needed. When health workers don’t understand the importance of disease surveillance, or don’t prioritize it, a key step is missed in timely identification of at-risk communities.
With USAID funding, MCSP mobilized to address this gap and the outbreak of vaccine-derived polio virus in Madagascar. Work began with supportive supervision visits to 13 health-facilities, including Dr. Famamesamtsoa’s health center, to assess the consistency and quality of AFP and VPD surveillance. MCSP and partners mentored the health workers and provided training and tools based on the assessments. The facilities are located in two regions – Diana and Sofia – in districts with higher numbers of children who have not completed their polio and other vaccines.
Providers were then monitored for their ability to identify AFP cases and take patient stool samples for laboratory testing within a two-week time period for virus detection. For Dr. Famamesamtsoa, it was highly motivating to understand that her efforts to improve local surveillance were integrally linked to the country’s efforts to eradicate polio.
Since these supportive supervision visits, Dr. Famamezamtsoa’s surveillance activities have increased significantly. She recently reported a suspected AFP case to the district level, following the necessary steps to ensure that the stool samples arrived in good condition for testing and remained engaged with the affected family until test results were available. Thankfully, in this case, the tests showed that the patient was negative for polio virus.
“Before the training, I did not take the time to identify AFP cases,” said Dr. Famamezamtsoa. “After learning how important the AFP surveillance component is to making Madagascar a polio-free country, I am motivated to actively search for cases.” Active surveillance takes place in the communities as well as when children are brought to the health facility for any reason.
Between 2014 and 2015, Madagascar had 11 confirmed cases of vaccine-derived poliovirus, signifying challenges with the immunization system that urgently needed attention. In response, the national Expanded Program on Immunization and partners concentrated on strengthening routine immunization activities and also implemented 13 national and subnational supplemental polio immunization campaigns. A series of five external outbreak response assessments were also conducted to identify and help the country address weaknesses in the immunization system.
By June 2018, these efforts and the diligence of individual providers like Dr. Famamezamtsoa led to an astounding achievement: Madagascar achieved Certification of Polio Eradication.
Eliminating polio in Madagascar is a key part of MCSP’s larger goal – contributing to the eradication of polio globally. From our collaboration in the historic, WHO-led global polio vaccine switch in April 2016, to the introduction and scale-up of inactivated poliovirus vaccine in 11 countries, we are “reaching the unreached” in even the most remote and marginalized communities.
The fight against polio can be won. But this requires continuous engagement with communities for joint problem identification, local ownership, and customized solutions. Local leaders and community members’ active involvement and ownership are of paramount importance to ensure that every child is vaccinated and that the country surveillance system can actively detect AFP and other VPD cases to prevent transmission and outbreaks.
By training providers in Madagascar to spread health messages on the importance of vaccination and conduct surveillance deep within their own communities, MCSP is building local resiliency against the return of polio – while also adapting this learning for emerging challenges like measles outbreaks. At-risk communities are increasingly knowledgeable about AFP and VPDs, and adept at identifying (and bringing to local health facilities) those children who show signs of paralysis.

