This blog originally appeared on The Huffington Post.
Palla Road village in Mahalapye Sub-District, Botswana is one of a growing number of communities where the USAID ASSIST project was invited to work with existing community structures and groups. With a small population of about 500, district officials identified the village as a “hot spot” in urgent need of joint community and facility efforts to improve care.
The local facility is a health post with two nurses and one health education assistant (HEA). Alongside members representing various village committees and groups, these two staff became the founding members of the 18-member community improvement team. The group chose the name Pusetso, which in Setswana means “restoration.”
Beginning in January 2016, the Pusetso team began exploring potential coordination roles of community structures to improve HIV-related services. After jointly analyzing the broader problems the village faced, the team prioritized the needs of sick community members, especially those patients deemed lost to follow-up. They committed to get them back to care, using existing community resources to help facility personnel in their mandate to find and reconnect with patients. ASSIST’s facilitation focused on guiding the team of community volunteers to focus their bimonthly discussions on simple but effective change ideas that have the potential to improve the quality and access of the community to patient-centered care.
From the beginning of their effort and discussions, Palla Road’s improvement team members recognized that confidentiality and disclosure of HIV status were very sensitive issues in the community. They knew they had to get creative, find “work-arounds”’ and ways to reinforce the trust of patients, and explore the reasons why people stopped seeking treatment at the facility.
However, first they needed to know how many members in their community might be affected. Following lively discussions, the team agreed that in order to preserve confidentiality, they would require only overall numbers of “lost patients” from the facility – not their names. This was sufficient for the purpose of monitoring the effect of their change ideas.

What change ideas did they produce with the help of the ASSIST improvement coaches? At the center of their idea was the recognition that actual patient follow-up needed to remain in the hands of formal health facility staff. This role falls specifically to the HEA as the public service cadre meant to strengthen the link between communities and facilities. As public servants subject to regular transfer policies, however, they often lack in-depth knowledge of the communities they serve.
The Pusetso team’s primary idea, therefore, was to support the HEA in her mandate by offering their local geographic knowledge to Palla Road’s wards and areas that allowed the facility staff to more easily locate and connect with patients. This way, the team offered its unique local knowledge while preserving existing public service guidelines and avoiding sensitive implications around confidentiality. Alongside this support to facility staff, the rest of the team spread messaging in the community that emphasized the need for its members to communicate with the facility in order to update files and prevent the future loss of patients.
Over the following weeks, the Pusetso team met twice a month, each time listening to updates from the health post staff on the progress with lost patients. By April 2016, the team proudly concluded that their combined change idea was successful, even though it was limited to one out of many related problems for the community.
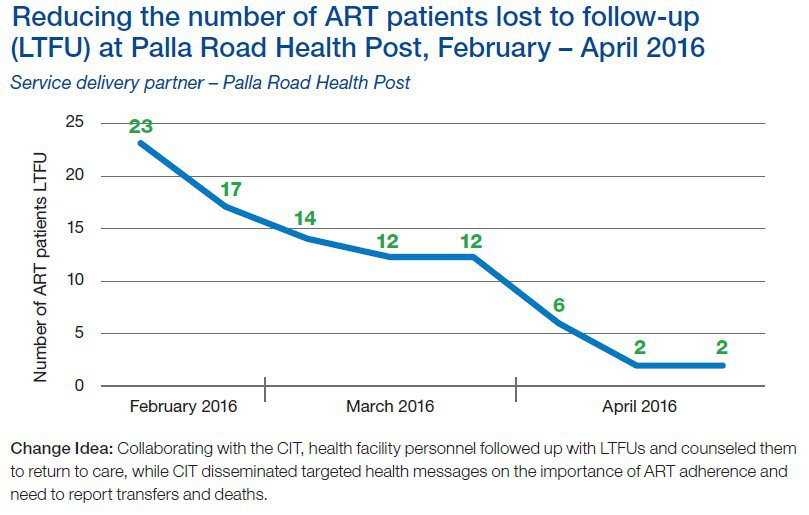
Nonetheless, for a small health post, the success of addressing their backlog in antiretroviral therapy patient management was an important one. It encouraged facility staff to build on this experience and institutionalize regular follow-up practices to prevent a new backlog. In addition, they began reorganizing their filing system for better continuous monitoring of all patients – those with HIV as well as other chronic care patients.
Overall, the experience in Palla Road demonstrates the potential role communities can play in improving community and facility collaboration. Senior managers from the District Health Management Team expressed interest in scaling up similar examples of improved collaboration, and strengthening the role of communities more broadly.
To read more about the experience of the Palla Road improvement team, click here.

